
C.A.R.E. (Clear Air, Respiratory Excellence) Project
Confirmation of COPD and asthma diagnosis with spirometry, evidence-based inhaler selection, and correct inhaler usage technique can benefit patients’ respiratory health and significantly reduce greenhouse gas emissions.
Authors

Carly Jones

Anna DiFrancesco
Summary
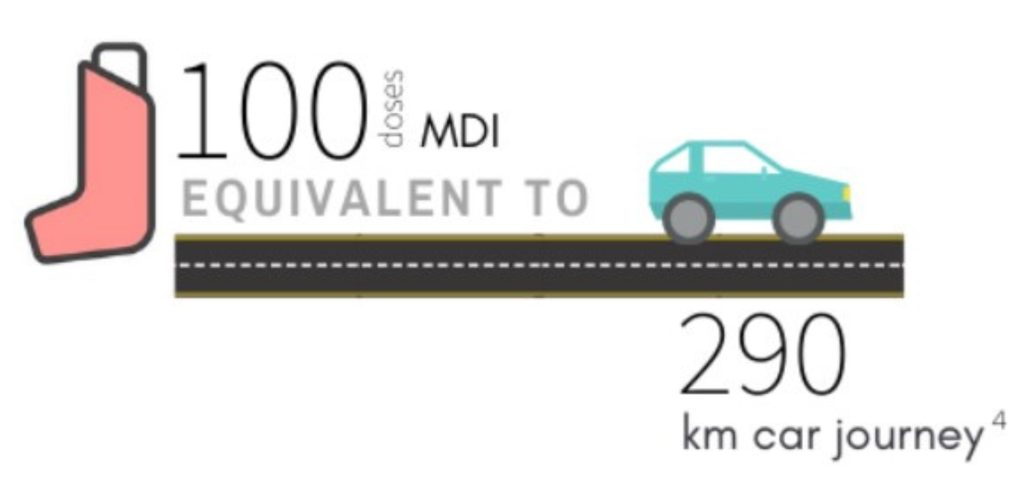
Metered dose inhalers (MDIs) are a significant source of healthcare’s carbon footprint.
Alternative: Dry Powder Inhalers (DPIs) have a smaller impact.
Section 1: Environmental Impact
The Carbon Impact of MDIs
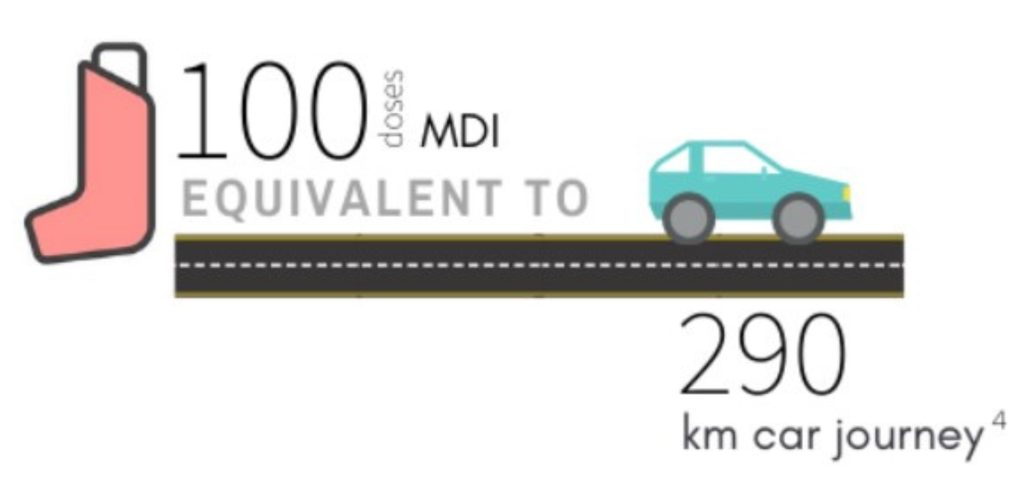
Metered dose inhaler (MDI) devices rely on propellants to deliver medication when the device is actuated.
These hydrofluorocarbon (HFC) propellants are 1300-3350 times more potent greenhouse gases than carbon dioxide. The propellants account for 90-98% of the global warming potential (GWP) of MDIs over their life cycle. (1) (appendix 1)
The propellants account for 90-98% of the global warming potential (GWP) of MDIs over their life cycle. (1)
The HFHT Green Team calculated Canadian emissions data from the life-cycle of inhalers (including waste impacts), which we used for the audit impact calculations (below). See Appendix E for those calculations.
The Relative Impact of Different Puffers:
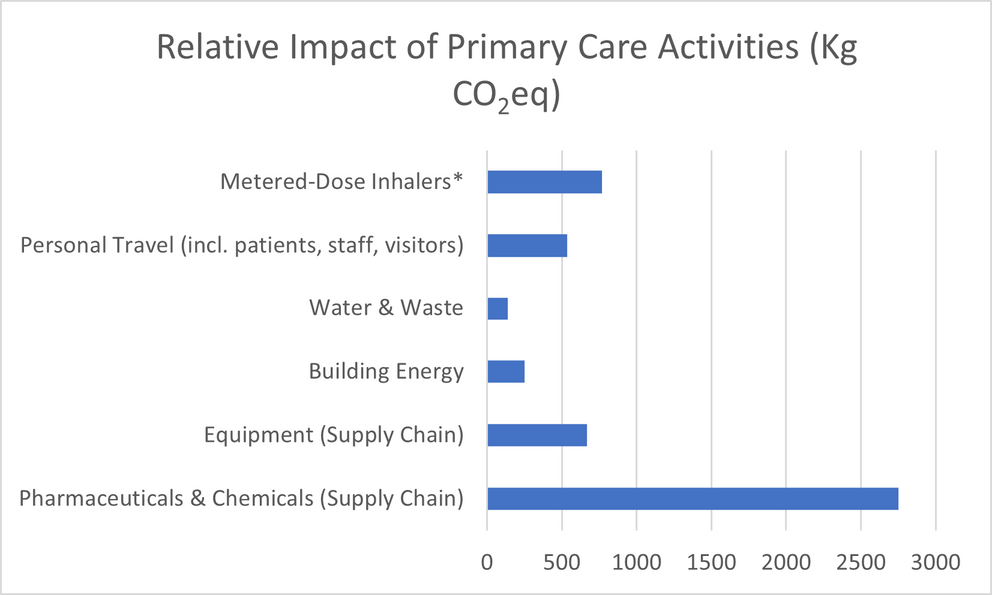
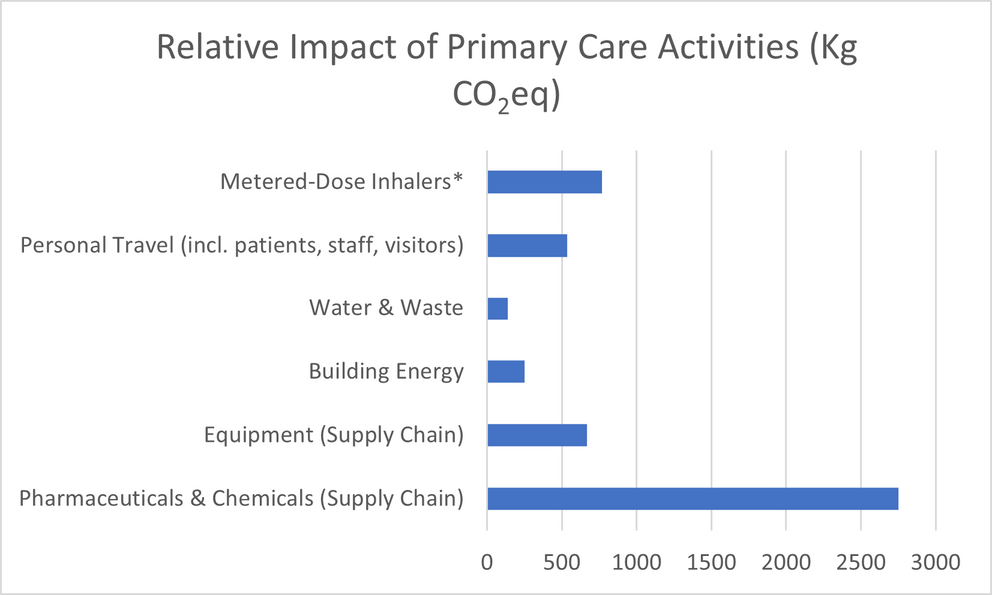
Metered-dose inhalers are estimated to contribute 3.1% of the carbon footprint of the National Health Service in the United Kingdom.
MDI Prescribing is Very Common in Canada.
MDI are a very commonly prescribed medication: ~900 000 salbutamol MDIs are distributed per month in Canada.
In Canada, approximately 9.5% of the population has an asthma diagnosis
Based on data from the U.K. in 2019
*In this study, MDI and anesthetic gas emissions were combined. However, in
primary care, MDI prescription far outweighs 4 anesthetic gas use.
Section 1: Recommendations
When clinically appropriate, consider Dry-Powdered Inhalers (DPIs), which have a lower carbon footprint compared to MDIs, even when including the impact of waste over each inhaler’s life cycle. (1,9)
See Appendix B for MDI alternatives including cost and ODB coverage.
“In many countries, like Finland and Sweden, good control of asthma and COPD is achieved at a national level while the majority of patients using inhaled therapies are treated with DPIs, (56% in Finland and 71% in Sweden).” (1,2)
Sometimes MDIs are necessary:
- Severe COPD
- Preschoolers
- Older age
- Financial/drug coverage issues
- Patient preference
- Insufficient inspiratory flow

Image Caption
Section 2: Confirming Diagnosis
The Carbon Impact of MDIs
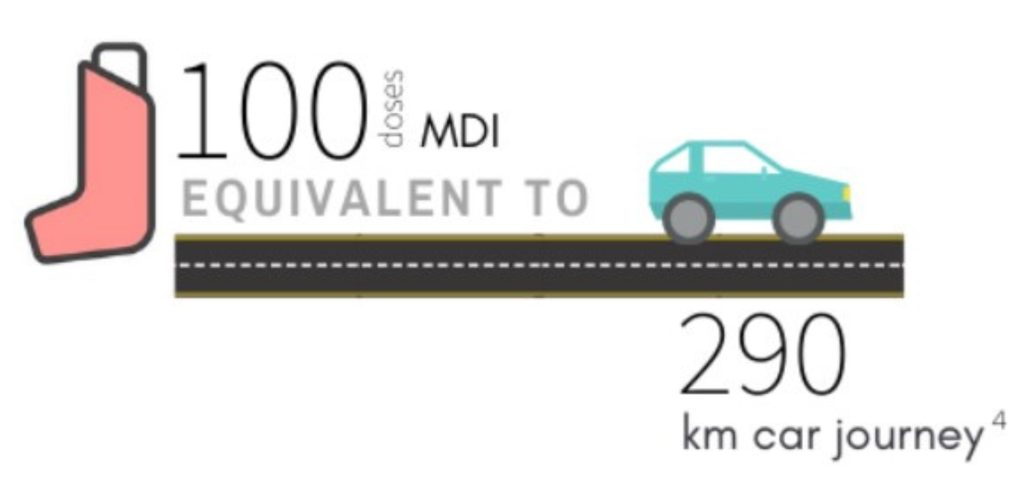
Metered dose inhaler (MDI) devices rely on propellants to deliver medication when the device is actuated.
These hydrofluorocarbon (HFC) propellants are 1300-3350 times more potent greenhouse gases than carbon dioxide. The propellants account for 90-98% of the global warming potential (GWP) of MDIs over their life cycle. (1) (appendix 1)
The propellants account for 90-98% of the global warming potential (GWP) of MDIs over their life cycle. (1)
The HFHT Green Team calculated Canadian emissions data from the life-cycle of inhalers (including waste impacts), which we used for the audit impact calculations (below). See Appendix E for those calculations.
The Relative Impact of Different Puffers:
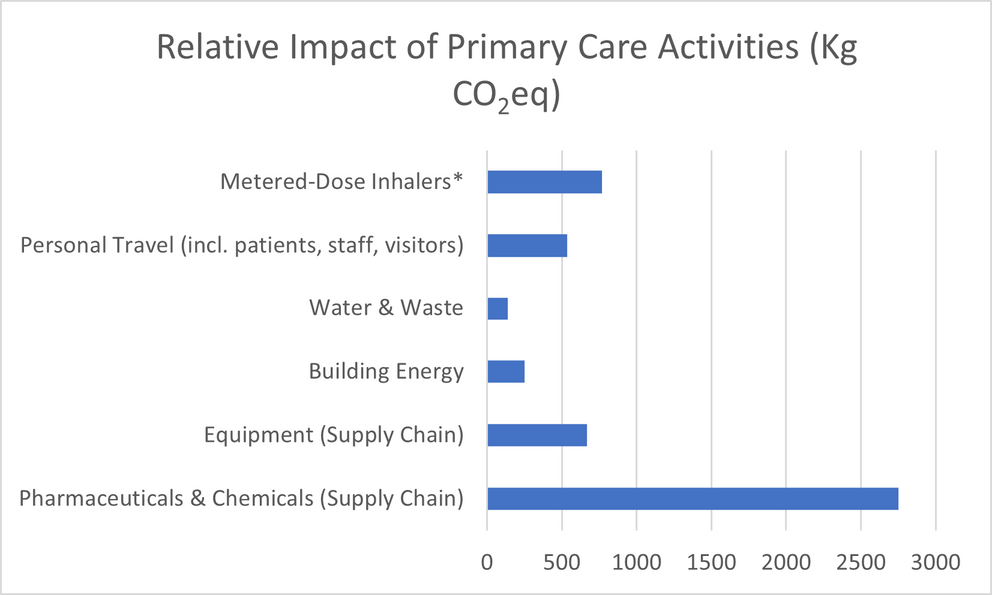
Metered-dose inhalers are estimated to contribute 3.1% of the carbon footprint of the National Health Service in the United Kingdom.
MDI Prescribing is Very Common in Canada.
MDI are a very commonly prescribed medication: ~900 000 salbutamol MDIs are distributed per month in Canada.
In Canada, approximately 9.5% of the population has an asthma diagnosis
Based on data from the U.K. in 2019
*In this study, MDI and anesthetic gas emissions were combined. However, in
primary care, MDI prescription far outweighs 4 anesthetic gas use.
Section 1: Recommendations
When clinically appropriate, consider Dry-Powdered Inhalers (DPIs), which have a lower carbon footprint compared to MDIs, even when including the impact of waste over each inhaler’s life cycle. (1,9)
See Appendix B for MDI alternatives including cost and ODB coverage.
“In many countries, like Finland and Sweden, good control of asthma and COPD is achieved at a national level while the majority of patients using inhaled therapies are treated with DPIs, (56% in Finland and 71% in Sweden).” (1,2)
Sometimes MDIs are necessary:
- Severe COPD
- Preschoolers
- Older age
- Financial/drug coverage issues
- Patient preference
- Insufficient inspiratory flow

Image Caption
Section 3: Action Plan
The Carbon Impact of MDIs
Metered dose inhaler (MDI) devices rely on propellants to deliver medication when the device is actuated.
These hydrofluorocarbon (HFC) propellants are 1300-3350 times more potent greenhouse gases than carbon dioxide. The propellants account for 90-98% of the global warming potential (GWP) of MDIs over their life cycle. (1) (appendix 1)
The propellants account for 90-98% of the global warming potential (GWP) of MDIs over their life cycle. (1)
The HFHT Green Team calculated Canadian emissions data from the life-cycle of inhalers (including waste impacts), which we used for the audit impact calculations (below). See Appendix E for those calculations.
The Relative Impact of Different Puffers:
Metered-dose inhalers are estimated to contribute 3.1% of the carbon footprint of the National Health Service in the United Kingdom.
MDI Prescribing is Very Common in Canada.
MDI are a very commonly prescribed medication: ~900 000 salbutamol MDIs are distributed per month in Canada.
In Canada, approximately 9.5% of the population has an asthma diagnosis
Based on data from the U.K. in 2019
*In this study, MDI and anesthetic gas emissions were combined. However, in
primary care, MDI prescription far outweighs 4 anesthetic gas use.
Section 1: Recommendations
When clinically appropriate, consider Dry-Powdered Inhalers (DPIs), which have a lower carbon footprint compared to MDIs, even when including the impact of waste over each inhaler’s life cycle. (1,9)
See Appendix B for MDI alternatives including cost and ODB coverage.
“In many countries, like Finland and Sweden, good control of asthma and COPD is achieved at a national level while the majority of patients using inhaled therapies are treated with DPIs, (56% in Finland and 71% in Sweden).” (1,2)
Sometimes MDIs are necessary:
- Severe COPD
- Preschoolers
- Older age
- Financial/drug coverage issues
- Patient preference
- Insufficient inspiratory flow

Image Caption
Section 1: Environmental Impact
The Carbon Impact of MDIs
Metered dose inhaler (MDI) devices rely on propellants to deliver medication when the device is actuated. These hydrofluorocarbon (HFC) propellants are 1300-3350 times more potent greenhouse gases than carbon dioxide. The propellants account for 90-98% of the global warming potential (GWP) of MDIs over their life cycle. (1) (appendix 1)
The propellants account for 90-98% of the global warming potential (GWP) of MDIs over their life cycle. (1)
Metered-dose inhalers are estimated to contribute 3.1% of the carbon footprint of the National Health Service in the United Kingdom. (3)
The Relative Impact of Different Puffers:
These are some Metered Dose Inhalers (10-28kg CO2 equivalents/inhaler ) available in Canada:
These are some Dry Powder Inhalers (0.5-1kg CO equivalents inhaler ) available in Canada:
For a quick overview of puffer categories see Appendix A from the Lung Association.
MDI Prescribing is Very Common in Canada
- MDI are a very commonly prescribed medication: ~900 000 salbutamol MDIs are distributed per month in Canada
- In Canada, approximately 9.5% of the population has an asthma diagnosis
Section 1: Recommendations
When clinically appropriate, consider Dry-Powdered Inhalers (DPIs), which have a lower carbon footprint compared to MDIs, even when including the impact of waste over each inhaler’s life cycle. (1,9)
See Appendix B for MDI alternatives including cost and ODB coverage.
“In many countries, like Finland and Sweden, good control of asthma and COPD is achieved at a national level while the majority of patients using inhaled therapies are treated with DPIs, (56% in Finland and 71% in Sweden).” (1,2)
Sometimes MDIs are necessary:
- Severe COPD
- Preschoolers
- Older age
- Financial/drug coverage issues
- Patient preference
- Insufficient inspiratory flow
To minimize carbon impact if MDIs are necessary:
a. Ensure proper MDI usage including a spacer device, which improves drug delivery and can therefore reduce amount needed. Refer to Section 2C for information on technique.
b. If salbutamol is needed as a reliever, consider prescribing Airomir MDI as that reliever (a specific generic of salbutamol) instead of other formats of salbutamol MDI when an MDI reliever is necessary (~1/3 of the carbon footprint of other salbutamol MDIs). On these prescriptions, write “dispense as written” so it is not switched to generic salbutamol or Ventolin.
c. Encourage patients to return their old inhalers to pharmacies for recycling and incineration. Compared to landfill disposal, this saves 4-18 kg CO (eq) per inhaler. See this link for a list of pharmacies accepting inhalers.
d. Clinicians can use an inspiratory flow check device to choose between MDI and DPI. You can order a C.A.R.E. Project Support Kit here, which includes DPI whistles for use with low- to average-risk patients. For high-risk patients (especially COPD), you may require an InCheck DIAL device to measure if they have a suboptimal peak inspiratory flow rate.
Section 2: Confirming Diagnosis
Part A: Ensure Accurate Diagnosis
Long-term inhalers are often prescribed for asthma and COPD without confirmation of diagnosis. We can avoid unnecessary puffer prescribing for asthma and COPD by
ensuring diagnosis with spirometry.
44% of Canadians who receive a diagnostic label of asthma have never had spirometry testing. Up to 67% of Canadians with COPD, chronic bronchitis, and emphysema have had no spirometry.
When the diagnosis is not confirmed, there is potential patient harm due to missed alternative diagnoses, (20,24) unnecessary medication costs (20-23, 24) and side effects, (20, 21,23, 24) and patients believing they have a chronic illness. (23)
Section 2A: Recommendations
Ensure accurate diagnosing of asthma and COPD using spirometry to avoid unnecessary MDI prescribing.
Diagnosing Asthma
Not all wheezes are due to asthma! In a large Canadian study, 33% of patients who had received a diagnosis of asthma from their physician in the last 5 years did not have asthma when assessed objectively with lung function tests. (21) However, 79% of these non-asthmatic patients were in fact using asthma medications. (21)
Guidelines uniformly recommend objective testing to establish asthma diagnosis. Cough, wheeze, or dyspnea can be caused by other conditions.
“Don’t initiate medications for asthma (e.g., inhalers, leukotriene receptor antagonists, or other) in patients ≥ 6 years old who have not had confirmation of reversible airflow limitation with spirometry, and in its absence, a positive methacholine or exercise challenge test, or sufficient peak expiratory flow variability.” ~Choosing Wisely (17)
The best time to perform spirometry is when the patient is symptomatic. Spirometry can generally be performed in children 6+ years of age.
In children < 6 years of age who are unable to perform spirometry, a trial of therapy (8–12 weeks in duration) and monitoring of symptoms can act as a surrogate method to diagnose asthma.
This recommendation may not be applicable in patients who cannot reproducibly undergo objective testing for asthma (including children less than 6 years old), and in settings where such testing is not available.
Diagnosing COPD
Not all shortness of breath, chronic cough, and sputum are COPD. Guidelines uniformly recommend objective testing to establish a COPD diagnosis.
“A diagnosis of COPD should be considered in any patient who has dyspnea, chronic cough, and/or sputum production and an appropriate history of exposure to noxious stimuli. However, not all patients with these symptoms have COPD, and a spirometry demonstrating a post-bronchodilator forced expiratory volume in one second to forced vital capacity (FEV1/FVC) ratio < 70% (or less than the lower limit of normal, if available) is required to make a definitive diagnosis.” ~ Choosing Wisely (17)
Viral Infections: How long should that cough last?
Adults: The majority of adults with a short duration of cough from an acute respiratory tract infection have a viral rather than a bacterial infection. Patients often underestimate the typical cough duration from an infectious illness. The average duration of cough (not treated with antibiotics) is around 18 days, though patients only expect to cough for 5 to 7 days. (30)
Children: The duration of normal paediatric acute cough can be 5-20 days, or 10-14 days on average. Several studies confirm that prescribing MDIs does not benefit these coughs:
“There is no evidence to support using beta-2-agonists in children with acute cough and no evidence of airflow obstruction.” (33)
Section 2B: New Asthma Treatment Guidelines
Asthma treatment guidelines (> age 12) have recently changed. (25,26)
“There is new evidence in children ≥12 years of age and adults that PRN budesonide/formoterol (bud/form) decreases exacerbations in comparison to PRN SABA, with different levels of evidence in those with very mild versus mild asthma.” (34)
Pilot Site Physician’s Example of Anti-Inflammatory Reliever Strategy:
*Symbicort is currently the only Canadian puffer with the evidence-based formoterol/budesonide combination. A generic is expected Fall 2022.
Reduce SABA Prescribing
“For safety, GINA no longer recommends treatment of asthma in adults and adolescents with Short-Acting Beta-2-Agonists (SABA) alone, without inhaled corticosteroids (ICS). There is strong evidence that SABA-only treatment, although providing short-term relief of asthma symptoms, does not protect patients from severe exacerbations, and that regular or frequent use of SABA increases the risk of exacerbations.” (25)
The Risks Associated with Frequent SABA overuse:
- Rebound Hyperresponsiveness (35)
- Decreased Broncho-protection (35)
- Decreased Bronchodilator Response (35)
- Increased Allergic Response (35)
- Increased Eosinophilic Inflammation (35)
- Increased E.D. presentations (36)
- Increased death rate from asthma (37)
According to 2020 SABINA studies, the use of more than 2 SABA inhalers per year (regardless of additional maintenance/controller medication (e.g. ICS)) is correlated with increased exacerbation and hospitalization incidence and mortality. (38,39)
Asthma Control with DPIs
ICS use is 73% higher when patients only have 1 inhaler (e.g. combined ICS/LABA).
With better asthma control (including maintenance therapy), fewer relievers are necessary because fewer exacerbations occur. (25, 27, 28, 41)
What is the Alternative?
For asthmatics aged 12+, GINA states:
“Every adult and adolescent with asthma should receive ICS-containing controller medication to reduce their risk of serious exacerbations, even patients with infrequent symptoms. Every patient with asthma should have a reliever inhaler for as-needed use, either low-dose ICS-formoterol or SABA. ICS-formoterol is the preferred reliever, because it reduces the risk of severe exacerbations compared with treatment options in which the reliever is SABA. However, ICS-formoterol should not be used as the reliever by patients who are taking a different maintenance ICS-LABA; for these patients, the appropriate reliever is SABA.” (25-26, 42-45)
CTS Guideline State:
“Individuals with well controlled asthma on no medication or PRN SABA at lower risk of exacerbation can use PRN SABA, daily ICS + PRN SABA, and if ≥ 12 years of age PRN bud/form*. Individuals at higher risk of exacerbation even if well-controlled on PRN SABA or no medication, and those with poorly-controlled asthma on PRN SABA or no medication should be started on daily ICS + PRN SABA. In individuals ≥ 12 years old with poor adherence despite substantial asthma education and support, PRN bud/form* can be considered.” (34)
The only current Canadian DPI containing budesonide/ formoterol is Symbicort. Formoterol provides immediate and longer-acting bronchodilation. (42-43, 46-48)
See pg. 3-4 of the Symbicort product monograph for indications and clinical use for asthma. (49) A generic format is expected Fall 2022.
The MDI Zenhale also contains an ICS/formoterol combination, although its use as a reliever has not been studied.
Preferred treatment is found using a step-wise approach (as shown in Appendix C) depending on severity, starting with low dose prn ICS-Formoterol. (25)
Section 2C: High Quality Low Carbon Care: Puffer Technique
Inhaler technique studies show that between 12-71% of the time, they are not used correctly. (50-54)
MDI administration misuse is even more common in older adults (79% conducting critical errors) (55) and children (97% misuse). (56)
Inhaler misuse is associated with:
- Increased hospitalization and Emergency Department visits (54, 57)
- Increased need for oral steroids and antimicrobials (50)
- Poor disease control (52, 57, 58)
- Decreased quality of life. (52, 59)
MDI Techniques:
Proper Technique (60-61):
- Shake inhaler before every actuation
- Breathe out
- Slow inhale (4-5s) with lips on inhaler while actuating medication
- Hold breath for 10s (adults)
- Wait >30s before next actuation
Common Errors (61):
- Actuate 2x in a row
- Inhaling too quickly
- Not using aerochamber/spacer device
DPI Techniques
Proper Technique (50, 62-63):
- Deploy medication/load device
- Breathe out away from device
- Quick & forceful inhaler (~2s) with mouth on device opening, inhaler must be upright
- Hold breath for 10s (adults)
Common Errors:
- Inhalation too slow/does not generate enough force (63)
DPIs are easier to use, tend to have fewer inhalation errors with use, and often contain dose counters. (64-68)
Section 2C: Puffer techniques Recommendations
When prescribing inhalers (MDI or DPI), review and encourage accurate technique, as well as proper frequency and dose. (62,69)
Section 3: Action Plan
Section 3A: Tools for Change
Engage the Healthcare Team:
Pharmacists, respiratory educators, MDs, nurse practitioners, physicians, registered nurses, physician assistants, and other allied healthcare providers.
If you have access to an in-house pharmacist, consider a referral when:
- Refills for MDI inhalers are required and a diagnosis is confirmed in adults
- A patient is ready or contemplating smoking cessation
- Inhaler technique assessment is required
If you have access to a respiratory educator, consider a referral for:
- All adolescents and adults with asthma or COPD
- Confirmation of a diagnosis
- Spirometry history review is required
- Inhaler technique assessment is required
Engage the Healthcare Team
The Respiratory Therapist/Certified Respiratory Educator with the pilot office is supplied by and works within the Best Care program. The educator is a highly valued member of our team for asthma and COPD care and a key part of the pathway for clinically appropriately inhaler prescribing with a focus on disease control and SABA/MDI overuse.
For Ontario primary care offices interested in hosting the Best Care program contact: bestcare@argi.on.ca.
More Tools for Change:
If you are a team with a respiratory educator, consider referral to the Respiratory Educators for:
- Patients with a confirmed diagnosis of Asthma or COPD that would benefit from further education
- Higher needs for ongoing care
- Interest in quitting smoking with enrolment in the STOP program
- Need for inspiratory effort testing
- Referral to the HFHT Respiratory Education program would also be of interest to offices that do not have access to Best Care or an HFHT pharmacist.
Educational Opportunities
- Centre for Sustainable Health Systems, Dalla Lana School of Public Health: Inhaler Community of Practice, including Climate Impact of Inhalers Webinar
- Hamilton Family Health Team: Recording of our Clean Air, Respiratory Excellence webinar
Print and put up our MDI Poster to encourage conversation about puffer prescriptions with patients.
Helping your patient quit smoking is good and green care. See our Smoking Cessation infographic which includes patient support links.
Make these sample templates for communication your own (Appendix D):
Template A: To pharmacist to stop MDI repeats
Template B: Ocean E-Form “Inhaler Prescription”
Template C: Internal to admin requesting appt with patient
Template D: Ocean E-Form “Inhaler Technique Link”
Resources for Staff and Patients Regarding Good Inhaler Use
- Canadian Lung Association: How to use various DPIs
- How to use Turbuhaler
- How to use MDI inhaler video
- How to use soft mist inhalers
EMR MDI Prescription Search
To conduct an MDI, you can use our pre-made search queries:
You can Contact the Green Team or your QI lead for details. For information on searching other EMRs, read this article. See our example audit below!
MDI Prescription Audit Example
The HFHT MDI team did primary care practice audits to investigate the extent of MDI prescription in Hamilton. (70)
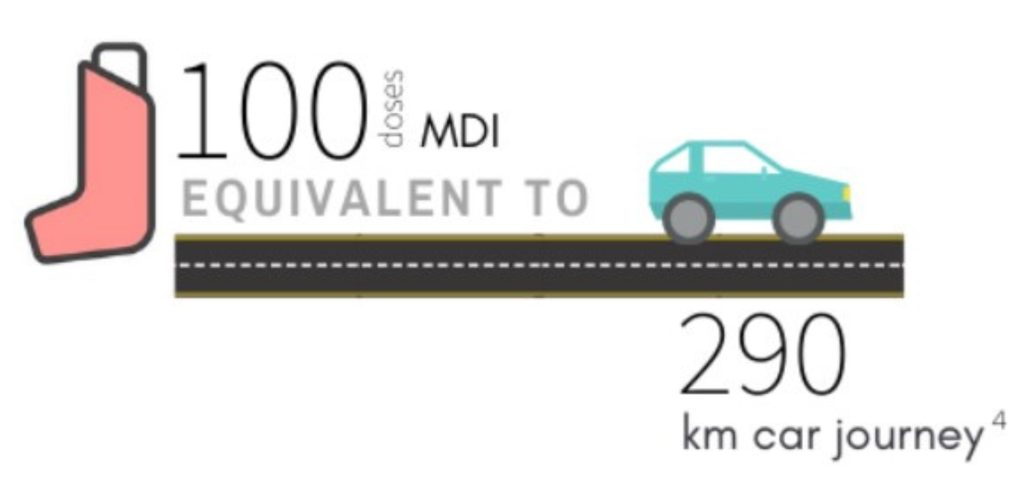
- A typical-sized practice (2000 patients) had, on average, 330 patients with an MDI prescription
- Assumptions: 1 inhaler/year/patient
- This represents ~9438kg of CO (eq) emissions/site/year
What we prescribe makes a difference.
The average primary care practice in our audit could cause emissions equivalent to 7.8 one-way car trips from Halifax to Vancouver a year via MDI prescriptions.
Section 3B: Pilot Site Tips for Success
Note: Our pilot site has access to an RN, pharmacist, and respiratory educator. We encourage providers with a team to engage their team’s scope of practice.
Observations from the Pilot Site
Patient preference and symptom control are prioritized when prescribing puffers. Puffer selection decisions are shared between provider and patient.
The most common opportunity to reduce MDI prescribing is when puffer prescriptions refills are requested from the pharmacy.
Patients are generally receptive to switching to PRN ICS/LABA strategy when clinially appropriate.
Having a confirmed diagnosis in a patient’s chart is key to avoiding unnecessary prescribing of any inhaler. We used our disease registry for this.
Approach the matter from a clinical perspective unless a patient brings up an environmental concern (e.g. review new GINA guidelines with patient so they know they can have better asthma control and less need for rescue meds).
ODB coverage can be a barrier (for example, some DPI relievers are not covered by ODB). Bricanyl Turbuhaler is covered.
Offer visits for inhaler technique review to assess patients’ inhalation technique from device and make suggestions/changes.
Have aids at your disposal to make the MDI to DPI transition smoother (e.g. demonstration devices, posters in clinical rooms).
Patients with confirmed diagnosis who are well-controlled with MDI strategy may not want to switch. Consider substituting Airomir MDI. It is an alternate form of salbutamol with 1/3 of the propellent and is covered under ODB, although patients may need to cover a $0.84 cost difference between this and generic salbutamol.
Patients who are currently on MDI therapy with prior unconfirmed diagnosis and no confirmatory testing may not feel comfortable coming off of their inhalers even if their (recent) spirometry and subsequent methacholine challenge test results are normal.
New Diagnosis of COPD/asthma:
Ensure accurate diagnosis with spirometry (and methacholine if necessary for asthma). Warn patients if tests are negative, they may get a call to discuss inhalers. Whenever clinically appropriate, the pilot site physician started newly-diagnosed patients on DPI over MDI.
Thank you for learning about sustainable inhaler prescribing that is:
- Patient-Centered
- Evidence-Based
- Multidisciplinary
- Low-Carbon
- Supported with tools/pathways